While satisfied patients consistently show better outcomes in psychiatric care[1],[2], less is known about whether being well-informed of rights contributes independently to clinical improvement – beyond the established effects of overall satisfaction.
To explore this, we examined inpatient admission-to-discharge Statistically Meaningful Improvement (SMI)[3] on three self-report clinical measures:
- BASIS-32[4] (N = 207,145), a measure of adult patient functioning
- PHQ-9[5] (N = 139,947), a measure of adult depression
- CABA-Y[6],[7] (N = 83,775), a measure of problem behaviors in adolescents aged 12 to 17
All patients, as part of the routine patient satisfaction survey process, responded to a single question assessing how informed they felt regarding their rights[8].
While being informed of rights is linked to better clinical improvement, the overall satisfaction context matters.
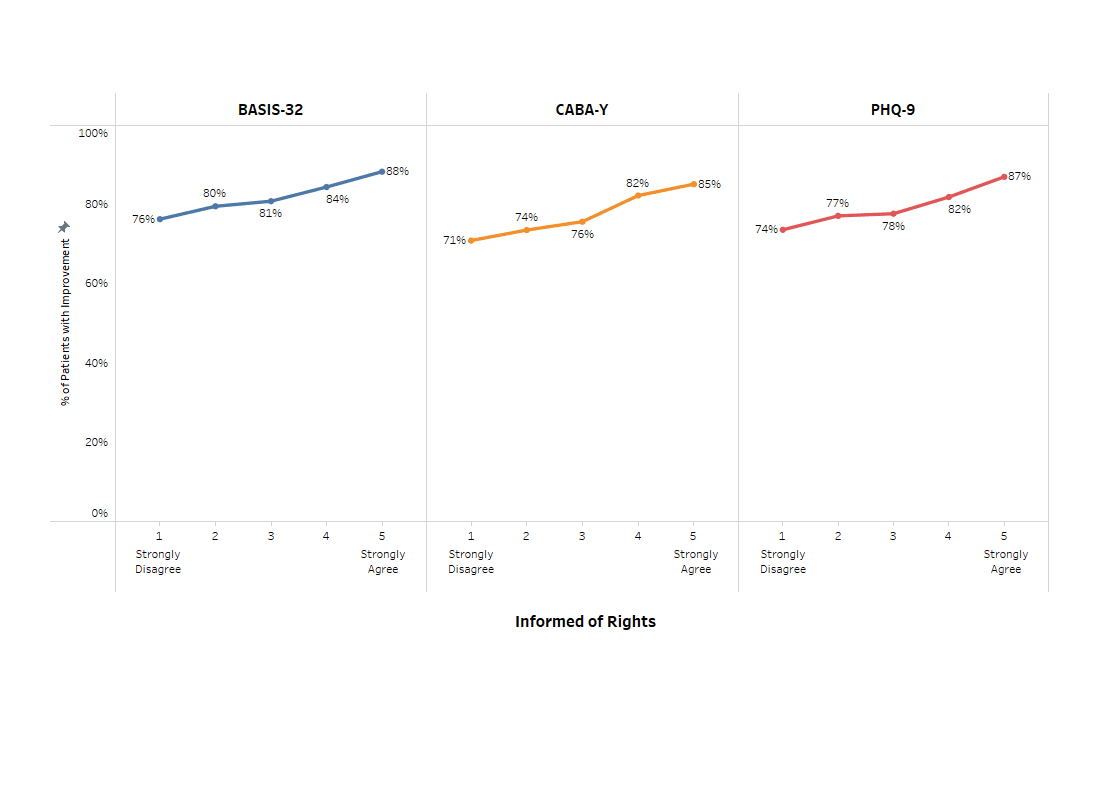
- By itself, being informed of rights and Statistically Meaningful Improvement had a small but positive association, where those more informed had better outcomes.
- Being informed of rights was also strongly associated with other satisfaction items.
- Once additional satisfaction items were considered, the link between informed of rights and clinical outcomes disappeared. In other words, among patients who are equally satisfied overall, those who feel more informed about their rights do not necessarily have better outcomes.
Figure 1. (Non-interactive) As ‘Informed of Rights’ increases, so does the percent of patients improving on clinical outcomes.
Implications for clinical practice
Informing patients about their rights is necessary but by itself insufficient – it should be embedded within the broader patient experience (e.g., staff, treatment, environment). Patients’ sense of control over their situation enables more active engagement in their treatment[9], and it may be that informing patients about rights[10] such as participation in treatment planning, refusing treatment within certain circumstances, having a safe environment and so on, can increase that sense of control. Moreover, the high correlation between informed of rights and other areas of patient satisfaction supports this. With this in mind, despite no direct, measurable impact on improvement, being informed of rights does seem to have an indirect impact on clinical improvement. Ultimately, being informed can play a role in the overall patient experience, and thereby in clinical improvement.
References
[1] Holcomb, W. R., Parker, J. C., Leong, G. B., Thiele, J. & Higdon, J. (1998). Customer satisfaction and self-reported treatment outcomes among psychiatric inpatients. Psychiatric services, 49, 929-934.
[2] Baradell, J. G. (1995). Clinical outcomes and satisfaction of patients of clinical nurse specialists in psychiatric-mental health nursing. Archives of Psychiatric Nursing, 9, 240-250.
[3] Note: SMI refers to a metric used to determine the degree of statistical change from admission to discharge. Based on the amount of change, patients are categorized into one of five SMI categories: Large improvement, small improvement, no effect, small decline, or large decline.
[4] BASIS-32: The Behavior and Symptom Identification Scale is a self-report measure of a patient’s functioning, rated on a scale of 0 “No difficulties” to 4 “Extreme difficulties”. BASIS-32 © Mclean Hospital, used by licensee with permission from Mclean Hospital.
[5] PHQ-9: The Patient Health Questionnaire is a self-report measure of a patient’s depression, rated on a Scale of 0 “Not at all” to 3 “Nearly every day”. Developed by Drs. Robert L. Spitzer, Janet B. W. Wiliams, Kurt Kroenke and colleagues, with an educational grant from Pfizer Inc.
[6] CABA-Y: The Child and Adolescent Behavior Assessment-Youth is a self-report structured questionnaire developed to assess problem behaviors during the past week, rated on a scale of 0 “No problem” to 3 “A big problem”.
[7] Morin, A.L., Miller, S.J., Smith, J.R., & Johnson, K.E. (2017). Reliability and validity of the Child and Adolescent Behavior Assessment (CABA): A brief structured scale. Child Psychiatry Hum Dev DOI, 48, 200-213.
[8] Informed of Rights was measured on a scale of 1 “Strongly Disagree” to 5 “Strongly Agree”.
[9] Odeh, A., Khayat, N., Abuzahra, S, Shaheen, A. & Nazzal, Z. (2024). Exploring patients’ rights awareness and implementations amongst hospitalized patients in Northern Palestine: insights from a local perspective. BMC Med Ethics, 25, 139.
[10] https://www.law.cornell.edu/uscode/text/42/9501