Reflections, MHO’s centralized online platform [1], has changed how our clients collect patient outcomes and satisfaction data. With a simple interface and workflows, it supports real-time data collection during patient assessments to inform treatment planning, track progress, and highlight areas of concern throughout a patient’s stay.
By 2025, all facilities transitioned to Reflections from legacy data collection systems such as Dynamic Forms and paper-based submissions. To evaluate the impact of this transition, we analyzed changes in data volume and quality across four of the most commonly used assessments:
- Behavioral and Symptom Identification Scale (BASIS-32) [2]
- Child and Adolescent Behavior Assessment–Youth (CABA-Y) [3]
- Patient Health Questionnaire-9 (PHQ-9) [4]
- Patient Satisfaction (PSF) [5]
Improvement in Data Capture
For consistency, the transition point was defined as the quarter when 80% of a facility’s data were submitted through Reflections.
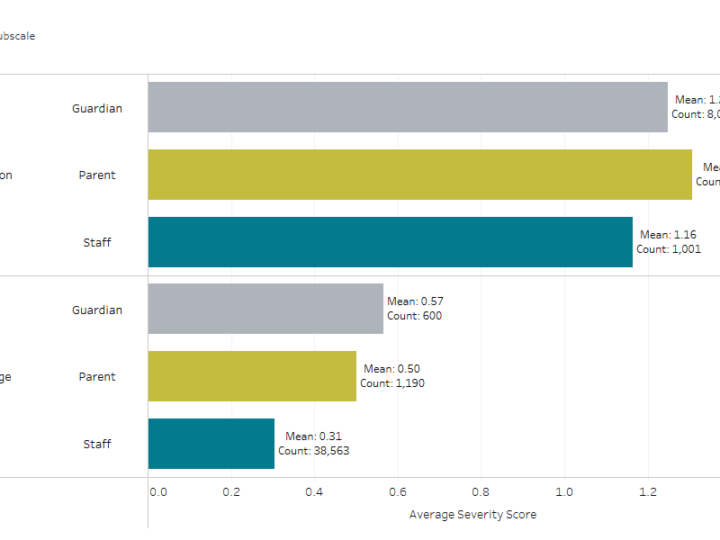
Following the transition, the rate of data capture — defined as the percentage of patients with valid, scorable assessments—increased from:
- 57% to 70% at admission
- 58% to 64% at discharge
That’s a meaningful boost in data volume resulting in increased opportunity to support individual patients’ treatment planning and progress monitoring as well as enhanced ability to evaluate program and facility effectiveness.
Figure 1. (Interactive) Data capture increased after transitioning to Reflections.
Data Quality
The shift away from paper forms contributed to a reduction in incomplete or invalid assessments. After discontinuing paper submissions, invalid assessments dropped from:
- 1.49% to 0.21% at admission
- 0.75% to 0.34% at discharge
Why It Matters
Access to complete and timely outcomes data allows for more informed treatment planning and enhanced monitoring of patient progress. It’s no wonder validated assessment tools have been linked to improved clinical outcomes and more effective care coordination[6].
Reflections plays a role in these improvements through:
- Increasing data capture
- Reducing invalid scores
- Supporting robust, data-driven insights for treatment planning
The usefulness of outcomes data extends beyond patient care, though. Even after patients discharge, their data helps facilities to identify strengths, address areas for improvement, and communicate performance to stakeholders including families, referral sources, and community partners. This contributes to ongoing quality improvement and transparency.
Additionally, larger and cleaner datasets enable stronger benchmarking. Facilities can compare performance across units or with peer organizations, helping guide strategic planning and goal setting.
Facilities seeking to improve data capture or expand how data are used in patient care, stakeholder reporting, or performance improvement efforts can reach out to [email protected] for support.
References
[1] Watts, Alex. “Introducing Reflections: Elevate Your Data Management and Boost Your Compliance Rates!” MHO, Mental Health Outcomes, 31 Jan. 2024, mhoutcomes.com/introducing-reflections/.
[2] BASIS-32: The Behavior and Symptom Identification Scale is a self-report measure of a patient’s functioning, rated on a scale of 0 “No difficulties” to 4 “Extreme difficulties”. BASIS-32 © Mclean Hospital, used by licensee with permission from Mclean Hospital.
[3] PHQ-9: The Patient Health Questionnaire is a self-report measure of a patient’s depression, rated on a Scale of 0 “Not at all” to 3 “Nearly every day”. Developed by Drs. Robert L. Spitzer, Janet B. W. Wiliams, Kurt Kroenke and colleagues, with an educational grant from Pfizer Inc.
[4] CABA-Y: The Child and Adolescent Behavior Assessment-Youth is a self-report structured questionnaire developed to assess problem behaviors during the past week, rated on a scale of 0 “No problem” to 3 “A big problem”.
[5] PSF: The Patient Satisfaction Form measures a patient’s overall satisfaction with the care they received in the program, rated on a scale from 1 (Poor) – 5 (Excellent).
[6] Johnston, Bradley C., et al. “Chapter 18: Patient-Reported Outcomes.” Cochrane, 2024, www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-18.